Recent events have placed an increasing emphasis on the importance of our psychological wellbeing. A pandemic, with lockdown, time away from education, work, friends and family has had wide-reaching impact, and this will be different for each of us. The World Health Organisation defines mental health as a state of wellbeing in which everyone can realise their own potential, cope with the usual stresses of life, work well and contribute to the community. NHS England explains 1 in 4 adults and 1 in 10 children experience mental illness. So how do we support each other and those in our wider circle?
Understanding how our mental health can be affected is important. Mental Health England give us a model for this – the Stress Container.
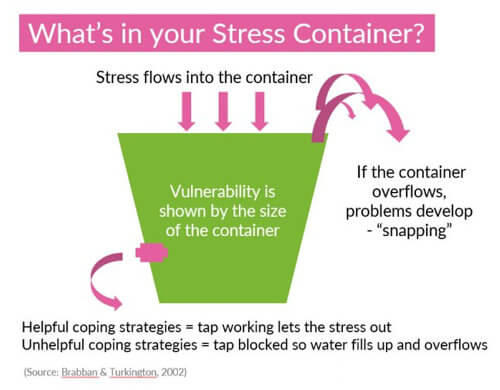
Imagine a container where ‘stress’ is added over time. Some of us have bigger containers than others, or the stress added might be a different size for me than it is for you. The container might keep filling up until it overflows and this is where problems can occur. My container may fill more quickly than yours. Now imagine there is a tap in the container which we can open or close. The tap might be blocked with ‘unhelpful coping strategies’ e.g. working harder, sleeping less, etc. But the tap can be opened with ‘helpful coping strategies’ e.g. time to self, exercise, fresh air, talking to someone. The most important thing is not to ignore it. You would not ignore a physical injury or illness so the same must apply to someone who may be struggling with mental health. There are lots of useful videos in the public domain that can be used appropriate to your context. I particularly like Talking Mental Health from the National Centre for Children and Families designed for a younger audience: https://www.youtube.com/watch?reload=9&v=nCrjevx3-Js
The BBC 3 Mental Health video series is also really useful for further insight – see the list of episodes at: https://www.bbc.co.uk/programmes/p06n93ys
Support Steps
1. The first step to supporting another is to notice changes. Is the individual unusually quiet, angry, despondent, busy, insular, tired, and so on?
2. The second step is to initiate a conversation. “I’ve noticed that you seem quieter than usual Dave. Would you like to talk it through? I’m available to listen.” Make sure you find a private space and that you allow time for the conversation. The person needs to feel comfortable to be able to talk. If they seem reluctant, you can ask if they have someone they can talk to and ask about how they might make this happen.
3. The third step is to listen. Be open and empathetic – take it seriously. Listening, giving your attention, and acknowledging the situation. Offering advice or problem solving is not helpful at this stage – you are simply there to listen. The advice I might have may not work for the individual or might seem too big a hurdle to them. Reassuring the individual that their feelings are common is very helpful as people can feel alone and isolated. Reassuring that there are many sources of support available is also helpful.
4. The fourth step is to ask if Dave if he has experienced anything like this before and to ask about previous coping mechanisms. Is there someone at home/work/school who can support? Where children or vulnerable adults are concerned there maybe safeguarding concerns and you should follow your organisational process in this instance.
5. The fifth step is linking to the support available. These might be on site, provided by work or education resources. You might also consider suggesting their GP. You can also link to online resources.
There are a huge range of mental health charities, organisations and support groups.
Many can be found on the NHS website at: https://www.nhs.uk/conditions/stress-anxiety-depression/mental-health-helplines/
Mind has a wealth of on-line resources and their helpline will provide support as well as link to more local services: https://www.mind.org.uk/information-support/helplines/
We hope you found this article useful. Do talk to us with any questions, comments or feedback.
By Wendy Strohm FCIPD
Senior Consultant
Trained as a Mental Health First Aider, with lived experience of a mental health diagnosis.